In the heart of the UK’s National Health Service (NHS), patient waiting times have consistently been a critical issue. With health services stretched thin, the challenge of reducing waiting times for care, especially in emergency departments and for elective surgery, has become more pressing. This article explores the most effective techniques for UK hospitals to minimize waiting periods, drawing on evidence from various studies and data.
The Current State of Patient Waiting Times in the NHS
Patient waiting times in the NHS are a persistent concern, affecting the overall quality of care. Recent data reveals that patients waiting for elective surgery and in accident and emergency (A&E) departments often experience significant delays. These waiting times not only impact patient satisfaction but also have serious implications for health outcomes.
Additional reading : What Are the Best Approaches for UK Telecom Companies to Expand 5G Coverage in Rural Areas?
A systematic review of studies on waiting times shows that delays in care can lead to deteriorated health conditions, increased anxiety among patients, and in some severe cases, worse medical outcomes. Emergency departments are particularly strained, with patients often facing prolonged wait times before receiving treatment.
Interestingly, while some countries have implemented effective health policies to manage waiting times, the UK still faces challenges. The NHS has implemented various strategies, but their effectiveness varies. Therefore, understanding evidence-backed methods to reduce waiting times is vital.
Also to discover : How Can UK Small Businesses Use Behavioral Economics to Improve Marketing Strategies?
Techniques for Reducing Waiting Times in Emergency Departments
Emergency departments (A&E) face unique challenges due to the unpredictable nature of patient arrivals and the severity of cases. Reducing waiting times in these settings requires a multifaceted approach.
Triaging and Resource Allocation
One effective technique involves improving triage systems to prioritize patients based on the severity of their conditions. Enhanced triage protocols ensure that those with life-threatening conditions receive immediate attention, while less severe cases are managed appropriately within a reasonable timeframe.
Allocating resources efficiently also plays a critical role. Studies have shown that hospitals with well-distributed staff and equipment are better able to handle surges in patient numbers. This includes having a sufficient number of nurses and doctors on duty, particularly during peak times.
Implementing Technology
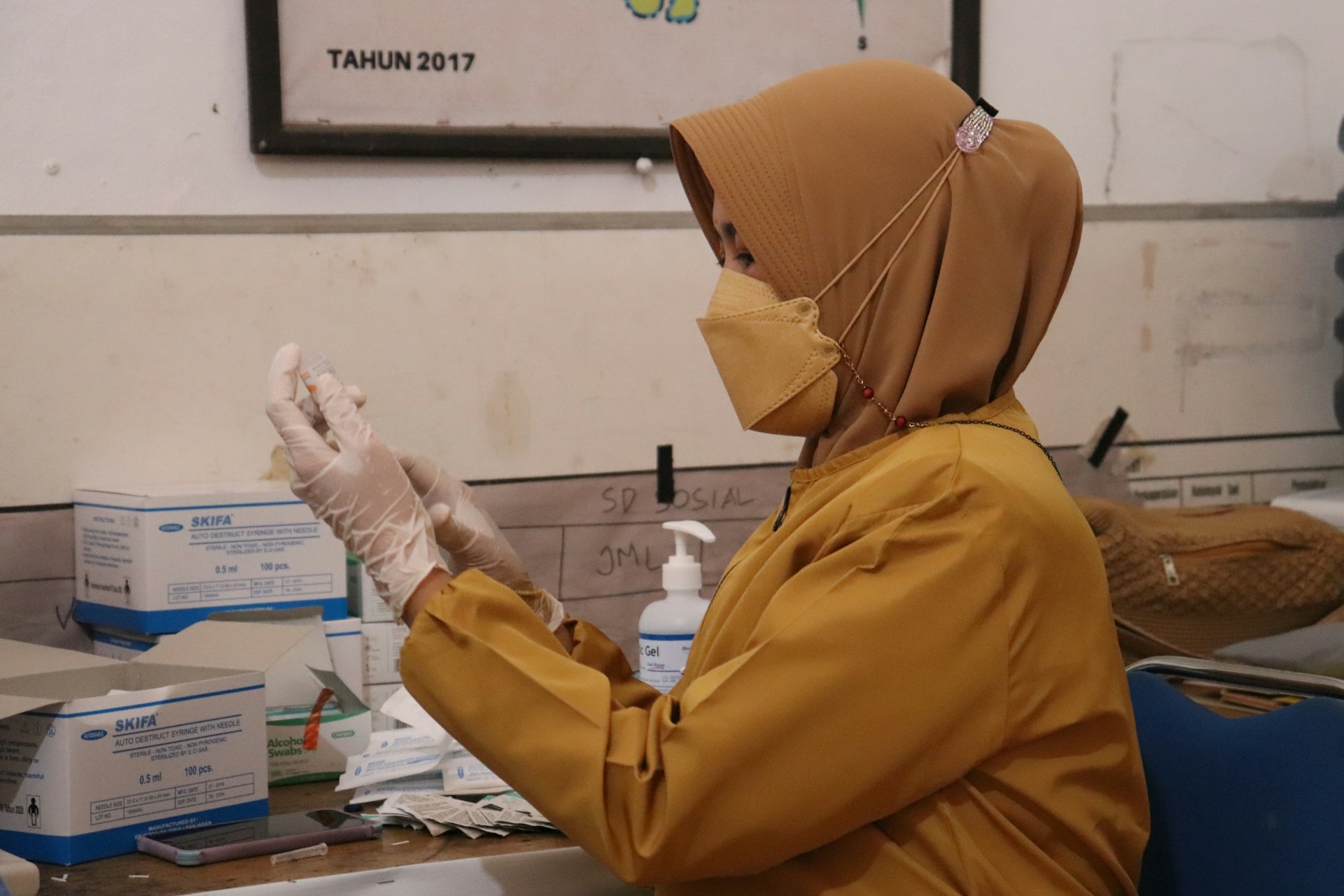
The use of technology in emergency departments can significantly reduce waiting times. Electronic health records (EHRs) streamline patient information management, allowing for quicker diagnosis and treatment. Moreover, digital check-in systems can reduce administrative bottlenecks, ensuring that patients are seen more quickly.
Telemedicine is another promising tool. For non-critical cases, virtual consultations can provide immediate care, freeing up emergency department resources for more severe cases. This approach has gained traction, particularly during the COVID-19 pandemic, showing consistent positive results in patient satisfaction and reduced waiting times.
Strategies for Minimizing Waiting Times for Elective Surgery
Elective surgery waiting lists are another significant challenge for the NHS. Prolonged waits for elective procedures can lead to worsened health conditions and increased patient frustration. Effective strategies are necessary to address these issues.
Scheduling Improvements
Improving scheduling practices is one of the most effective ways to reduce waiting times for elective surgery. This includes optimizing operating theatre schedules and ensuring that surgeries are scheduled based on urgency and available resources. Data from several hospitals show that better scheduling can lead to a significant reduction in waiting times.
Utilizing Data and Analytics
The NHS can leverage data analytics to predict and manage patient flow better. By analyzing historical data, hospitals can foresee periods of high demand and plan accordingly. This proactive approach helps in avoiding backlogs and ensures that operating theatres are used efficiently.
Collaborations and Partnerships
Collaborations with private health care providers can also alleviate the pressure on NHS hospitals. By outsourcing some elective surgeries to private facilities, the NHS can reduce waiting lists and ensure timely care for patients. This approach has shown limited but promising results in various health systems globally.
The Role of Health Policy in Reducing Waiting Times
Health policy plays a crucial role in shaping how waiting times are managed. Policies that incentivize efficiency and penalize delays can drive improvements in how hospitals operate.
National Targets and Accountability
Setting national targets for waiting times and holding hospitals accountable for meeting these targets is an effective policy measure. For instance, the NHS has targets for maximum waiting times in A&E and for elective surgery. Consistently measuring performance against these targets and addressing underperformance ensures that hospitals remain focused on reducing waits.
Investing in Health Services
Investment in health services, including infrastructure, technology, and personnel, is essential. Adequate funding allows hospitals to expand capacity, hire more staff, and invest in new technologies that can reduce waiting times. Studies have shown that countries with better-funded health systems generally have shorter waiting times.
Continuous Monitoring and Improvement
Continuous monitoring and improvement are key to ensuring that health policies remain effective. Regular audits and reviews help in identifying areas of improvement and implementing necessary changes. This dynamic approach ensures that policies evolve with changing circumstances and challenges.
Evidence-Based Approaches and Their Effectiveness
Drawing on evidence from systematic reviews and studies, several approaches have been identified as consistently effective in reducing patient waiting times.
Comprehensive Care Coordination
Comprehensive care coordination involves managing a patient’s entire care journey efficiently. This includes timely referrals, follow-ups, and ensuring that all parts of the healthcare system work seamlessly together. Evidence shows that effective care coordination can reduce waiting times and improve patient outcomes.
Patient Education and Communication
Educating patients about the care process and communicating clearly about expected wait times can improve patient satisfaction, even if the waiting period is longer than desired. When patients understand the reasons for delays and what to expect, they are more likely to be patient and satisfied with their care.
Multi-Disciplinary Teams
Utilizing multi-disciplinary teams to manage patient care can lead to more efficient use of resources and reduced waiting times. These teams bring together different healthcare professionals, ensuring comprehensive and timely care for patients.
Reducing patient waiting times in UK hospitals is a complex but achievable goal. By leveraging technology, improving scheduling and resource allocation, and implementing effective health policies, hospitals can make significant strides in reducing delays. Evidence from various studies and data highlights that a multi-faceted approach, involving both operational improvements and policy initiatives, is key to achieving this goal.
Ultimately, the NHS must continuously adapt and innovate to meet the evolving demands of healthcare. With the right strategies in place, patient waiting times can be minimized, leading to improved health outcomes and greater patient satisfaction. The consistent positive evidence from around the world suggests that with commitment and the right techniques, the NHS can effectively manage and reduce waiting times, ensuring timely and quality care for all patients.